UNDERSTAND AK
When thinking about sun damage, you may think of sunburn as it is, characteristically, a physical, painful burn.1,2 Whilst sunburn is one type of sun damage, it is important to remember that generally sun damage is not always visible and does not look the same for all skin types.1–3
Over time, everyone, no matter what their skin tone, can experience a build-up of sun damage. For some, this repeated damage can cause actinic keratosis (AK) patches (also referred to as solar keratosis or actinic damage) to develop on the skin – if left untreated, these patches have the potential to develop into skin cancer.3–5
Although more common in people with fair skin, anyone can develop AK patches:7

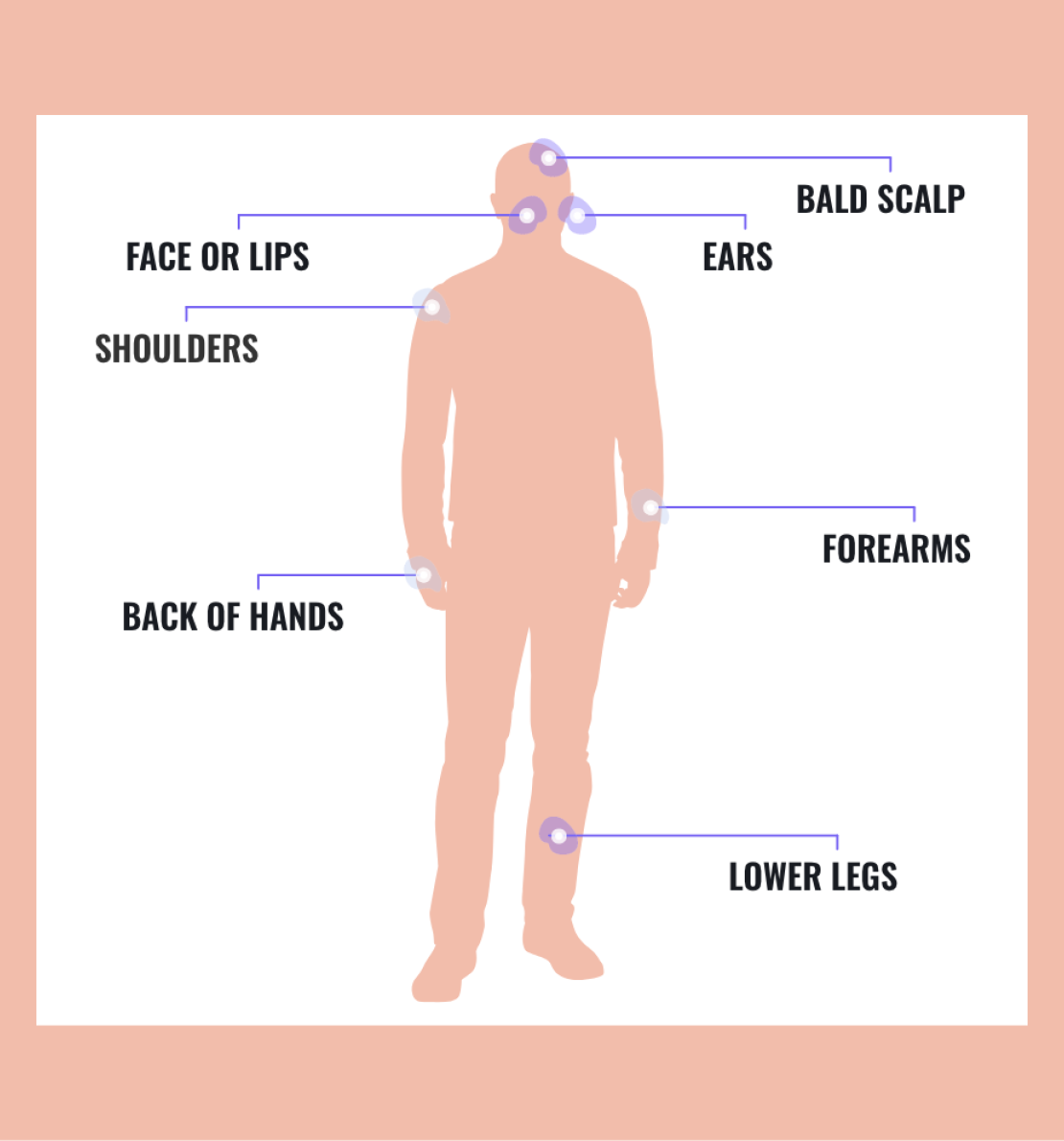
AK patches typically appear on the parts of the body that have had the most sun exposure.4,5,8–10
WHAT CAN AK PATCHES LOOK LIKE?
An AK patch can look rough, dry and/or scaly. These patches may:5,8,11,12
- Feel itchy
- Be flat or slightly raised
- Feel dry, rough, and scaly (like sandpaper)
- Vary in size from a few millimetres to 2cm (but they can be larger)
- Be the same color as the skin or can range from pink to red to brown
Having two or more visible AK patches can suggest underlying damage to the skin, which can mean an increased chance of developing skin cancer.9,10
Although AK patches can keep coming back, there are treatment options available as well as ways to prevent further sun damage that may be helpful.4,8,13
If AK patches are left untreated, they can potentially progress to a type of skin cancer called non-melanoma skin cancer (NMSC) which includes squamous cell carcinoma (SCC) and basal cell carcinoma (BCC).4,11,16
It is important to regularly check your skin for anything that is:17–21

You can do this at home by performing a skin check once a month, but it is generally recommended you visit a healthcare professional or dermatologist annually.17,20,22
When checking your skin it's important to know where to look.
Common sun-exposed areas of skin where AK patches could be found include:8,23
REGULARLY CHECK YOUR OWN SKIN FOR ANY SIGNS OF SUN DAMAGE AND POSSIBLE AK PATCHES
Make sure to speak with a healthcare professional or dermatologist if you are concerned or notice anything unusual on your skin.
KNOW YOUR AK RISK FACTORS
UV rays come from the sun but can also come from artificial sources such as tanning beds.24,25 Over time, these rays have the ability to damage skin cells which can lead to the development of both AK patches and skin cancer.24,25
There are different types of UV rays: UVA rays associated with causing signs of aging, UVB rays associated with causing sunburn and then UVC rays which are absorbed by the earth’s atmosphere and are not associated with damaging the skin.26,27
Both UVA and UVB rays damage skin cells which can lead to the development of skin cancer, so it is important to ensure you are protecting your skin.26
Everyone can be affected by sun damage, but some factors can put people at a higher risk.19,29–31
The risk of developing AK increases depending on factors such as:



WHY DOES A WEAKENED IMMUNE SYSTEM INCREASE THE RISK?
AK patches are more common in people who are immunosuppressed because their immune system’s ability to defend their body is weakened.11,36,37,39
IF YOU THINK YOU COULD BE AT A HIGHER RISK OF DEVELOPING AK PATCHES, VISIT A HEALTHCARE PROFESSIONAL OR DERMATOLOGIST.
LEARN HOW TO PREVENT AK
When it comes to looking after the skin, sun damage is preventable.8,27 To prevent sun damage and AK patches progressing to skin cancer, it is important to recognize any changes on your skin.21,39 AK patches will look different on all skin types.5,8,28,40 If you are concerned, please seek advice from a healthcare professional, dermatologist or pharmacist.
The risk of sun damage and developing AK patches can be reduced by minimizing how much time you spend in the sun and by protecting your skin.5,19
Follow the top 5 tips below to help protect your skin:
- Avoid peak sun hours (10–4pm) – this is when the sun’s intensity is highest25,41
- Wear protective clothing – dark-colored and thick items of clothing will help to prevent the sun’s UV rays from reaching your skin; appropriate hats can also help to protect your face, ears and neck25,41
- Stay in the shade – when possible, avoid direct sunlight25,41
- Avoid artificial sunlight (such as tanning beds that use UV light)25,41
- Wear sunscreen every day – and re-apply sunscreen throughout the day; even if the weather is cloudy or you are indoors. This is because the UV rays can still reach you in the shade or through windows and damage your skin18,28,41
Most sunscreens protect your skin against UVB rays, but only some protect you from UVA rays as well – this feature in sunscreens can be referred to as broad spectrum protection.18,41 When finding the right sunscreen, it is important to understand certain product features.
Some features that you may want to consider when looking for a sunscreen include:

To help you find the right sunscreen that will help you protect your skin and prevent sun damage build up…
ask a healthcare professional, dermatologist or pharmacist for one with the features that matter most to you
With a better understanding of AK, the signs you should look for, and how to properly protect yourself from the sun - you are now #AKaware.
Share this website with family and friends so they can become #AKaware too.
QUESTIONS & ANSWERS
WILL MY AK PATCHES TURN INTO SKIN CANCER?
Around 10% of AK patches will develop into skin cancer.23 However, you cannot identify which AK patches will become cancer and which will not, so it is recommended that all AK patches should be treated by a healthcare professional. 4,11,44,45
HOW CAN AK OR SKIN CANCER BE PREVENTED?
With AK being the No.1 most common pre-cancerous skin disease, protecting yourself from sun damage is key in the prevention of AK patches and the further damage that leads to skin cancer.8,46,47 There are a number of ways you can protect your skin, find out more by reading our sun safety tips.
CAN AK AND SKIN CANCER BE CURED?
Although AK patches are chronic, they are highly treatable and there are a number of different options to help you manage them.4,8 Similarly, when it is caught early, skin cancer is also highly treatable.21,39 To help you take care of your skin and discuss any concerns you may have about AK patches or skin cancer, make an appointment to speak with a healthcare professional or dermatologist.
WHAT SHOULD I DO IF I SEE SOMETHING THAT IS NOT NORMAL ON MY SKIN?
It is important to keep track of any abnormalities on your skin by doing regular skin checks.20,21 If you are seeing something unusual, new, or changing on your skin, speak to a healthcare professional or dermatologist.
Footnotes
*To reach the protection level indicated by the SPF, sunscreen products have to be applied in quantities similar to the ones used for testing, i.e., 2mg/cm2, which equals 6 teaspoons of lotion (approx. 36 grams) for the body of one average adult person.42
Abbreviations
AK, actinic keratosis; BCC, basal cell carcinoma; NMSC, non-melanoma skin cancer; SCC, squamous cell carcinoma; SPF, sun protection factor; UV, ultraviolet.
References
1. Skin Cancer Foundation. Skin cancer prevention. Available at: https://www.skincancer.org/skin-cancer-prevention/. Date accessed: April 2023. 2. Yale Medicine. Photoaging (sun damage). Available at: https://www.yalemedicine.org/conditions/sun-damage. Date accessed: April 2023. 3. American Academy of Dermatology Association (2022). How to spot a precancerous growth on your skin. Available at: https://www.aad.org/public/diseases/skin-cancer/find/at-risk/precancerous-growth. Date accessed: April 2023. 4. Cramer P and Stockfleth E. Expert Opin Emerg Drugs. 2020;25(1):49–58. 5. Casari A, et al. Biomedicines. 2018;6(1):8. 6. Shergill B, et al. Patient Prefer Adherence. 2013;8:35–41. 7. Skin Cancer Foundation. Actinic keratosis risk factors. Available at: https://www.skincancer.org/skin-cancer-information/actinic-keratosis/causes-and-risk-factors/#:~:text=Although%20anyone%20can%20develop%20AKs,higher%20risk%20for%20developing%20AKs. Date accessed: April 2023. 8. Skin Cancer Foundation. Actinic keratosis overview. Available at: https://www.skincancer.org/skin-cancer-information/actinic-keratosis/. Date accessed: April 2023. 9. Steeb T, et al. J Clin Med. 2020;9:1438. 10. Emre S. World J Dermatol. 2016;5(2):115–24. 11. Cohen J.L. J Clin Aesthet Dermatol. 2010;3(6):39–44. 12. Moy R.L. J Am Acad Dermatol. 2000;42:8–10. 13. Dianzani C, et al. Int J Dermatol. 2020;59(6):677–84. 14. Skin Cancer Foundation (2021). UV Radiation & Your Skin. Available at: www.skincancer.org/risk-factors/uv-radiation/. Date accessed: April 2023. 15. Rocholl M, et al. J Occup Health. 2020;62:e12083. 16. Skin Cancer Foundation (2022). Actinic keratosis warning signs. Available at: www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-warning-signs-and-images/. Date accessed: April 2023. 17. Yale Medicine. Actinic keratosis fact sheet. Available at: www.yalemedicine.org/conditions/actinic-keratosis. Date accessed: April 2023. 18. Skin Cancer Foundation (2021). Sun Protection. Available at: www.skincancer.org/skin-cancer-prevention/sun-protection/. Date accessed: April 2023. 19. Skin Cancer Foundation. Early Detection: Overview. Available at: https://www.skincancer.org/early-detection/. Date accessed: April 2023. 20. American Cancer Society. How to do a skin self-exam. Available at: https://www.cancer.org/healthy/be-safe-in-sun/skin-exams.html. Date accessed: April 2023. 21. Skin Cancer Foundation. Self Exams. Available at: https://www.skincancer.org/early-detection/self-exams/. Date accessed: April 2023. 22. Skin Cancer Foundation. Annual Exams. Available at: https://www.skincancer.org/early-detection/annual-exams/. Date accessed: April 2023. 23. Fuchs A and Marmur E. Dermatol Surg. 2007;33(9):1099–101. 24. Worldwide Cancer Research (2022). How does the sun cause cancer? Available at: https://www.worldwidecancerresearch.org/news-opinion/2022/march/how-does-the-sun-cause-skin-cancer/. Date accessed: April 2023. 25. News In Health (NIH). Sun and Skin (2014). Available at: https://newsinhealth.nih.gov/2014/07/sun-skin. Date accessed: April 2023. 26. Yu, S and Lee, S. Molecular & Cellular Toxicology. 2017;13:21–28. 27. American Cancer Society. Does UV Radiation Cause Skin Cancer? Available at: https://www.cancer.org/healthy/cancer-causes/radiation-exposure/uv-radiation.html. Date accessed: April 2023. 28. Chetty P, et al. Dermatol Ther (Heidelb). 2015;5(1):19–35. 29. Skin Cancer Foundation. The Sun Keeps Rising: Why Seniors Can’t Skip UV Protection. Sun & Skin News. Available at: https://www.skincancer.org/blog/the-sun-keeps-rising-why-seniors-cant-skip-uv-protection/. Date accessed: April 2023. 30. NIH National Cancer institute. Sunlight. Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/sunlight. Date accessed: April 2023. 31. Health and Safety Executive. Outdoor workers and sun exposure. Available at: https://www.hse.gov.uk/skin/employ/sunprotect.htm. Date accessed: April 2023. 32. Fors M, et al. BMC Dermatology. 2020;20(11):1–6. 33. Vimercati L, et al. Int J Environ Res Public Health. 2020;17(7):2321. 34. John SM, et al. J Eur Acad Dermatol Venereol. 2016;30 Suppl 3:38–45. 35. Hussain SK, et al. J Invest Dermatol. 2009;129(9):2142–7. 36. Mittal A, et al. Am J Transplant. 2017;17:2509–30. 37. Skin Cancer Foundation (2016). After a transplant: new dangers. Available at: www.skincancer.org/blog/after-a-transplant-new-dangers/. Date accessed: April 2023. 38. Didona D, et al. Biomedicines. 2018;6(1):6. 39. DermNet NZ (2016). Self skin examination. Available at: https://dermnetnz.org/topics/self-skin-examination. Date accessed: April 2023. 40. Guideline for the management of Actinic Keratoses. European Dermatology Forum 2011. Available at: http://www.euroderm.org/images/stories/guidelines/guideline_Management_Actinic_Keratoses-update2011.pdf. Date accessed: April 2023. 41. CDC. Sun Safety. Available at: https://www.cdc.gov/cancer/skin/basic_info/sun-safety.htm. Date accessed: April 2023. 42. Official Journal of the European Union. Commission recommendation of 22 September 2006 on the efficacy of sunscreen products and the claims made relating thereto. Available at: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2006:265:0039:0043:en:PDF. Date accessed: April 2023. 43. Pinto D, et al. J Investig Med. 2022;70(1):92–8. 44. Skin Cancer Foundation (2021). Is Actinic Keratosis Skin Cancer? Available at: www.skincancer.org/blog/is-actinic-keratosis-skin-cancer/. Date accessed: April 2023. 45. American Academy of Dermatology Association. How can I tell if I have skin cancer? Available at: https://www.aad.org/public/diseases/skin-cancer/find/know-how. Date accessed: April 2023. 46. Reinehr CPH and Bakos RM. An Bras Dermatol 2019;94(6):637–57. 47. Ferrándiz C, et al. Actas Dermosifiliogr. 2017;108(1):31–41.